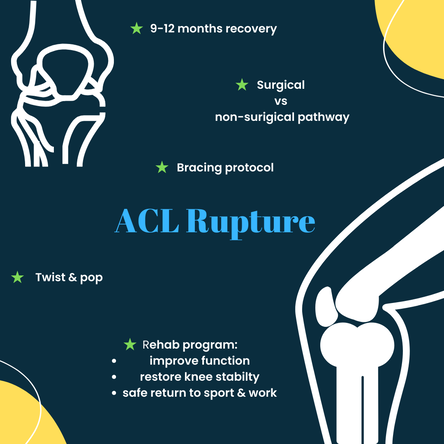
 It’s the dreaded feeling - the twist, the pop, the pain and the wobbly knee…. Many people have heard about people rupturing their ACL and the subsequent discussions about surgery, rehab and time off sport (hear.. “season-ending injury“) but do we actually know the best way to get that knee back to normal? The anterior cruciate ligament (ACL) provides stability through the knee connecting the femur (thigh bone) and the tibia (shin bone). It achieves this by preventing the sliding, gliding and rotating of the knee joint. If you tear your ACL your knee may become swollen, painful and feel weak or give way. The goal of any treatment program is to restore knee stability, improve function and for a safe return to sport, work and other activities. In the past we believed that to achieve a good outcome and to get back to pivoting sports (including that social touch footy game), an ACL reconstruction was required. Usually, an MRI, a referral to an orthopaedic surgeon and a physio follow the injury in various orders. And traditionally most active people have undergone an ACL Recon +/- prehab beforehand and a 9-12 month rehab program afterwards. Recent research has demonstrated that this “rule” of most people requiring a recon may need to be rethought…. A new insight into ACL rehab There have been a number of research projects and documented instances of ACLs healing and /or people returning to their previous activities (including Elite sports people) without undergoing an ACL recon and doing Rehab alone. !!! The issue is we don’t really know just from scanning who will respond well to rehab without surgery and those who most likely need surgery. The general consensus is that an initial 3-month Rehab program with or without a bracing protocol (chat to your health provider about this #crossprotocol #richardsonprotocol ) will give your ACL the chance to heal (and quite a % do) and to see if you will cope without the need for surgery. Regardless of surgery or no surgery , you will need to undertake a full comprehensive program over the next 9-12 months and pass the return to sport tests. The best thing is that if surgery IS required, and you’ve done the early work your outcomes after surgery are improved, your muscles will be stronger, you should have good movement, and all the bleeding and swelling will be gone. Now let’s answer some questions about the rehab alone option … Will my knee be “Stuffed” if I don’t get that early surgery? Studies have shown that there is very little difference in outcomes between ACL reconstruction surgery and rehab without surgery. Both treatment options result in similar levels of:
Can I return to sport? About half of all people with an ACL injury will return to the same level of sport, and this is the same whether they choose ACL surgery or rehab without surgery The most common reason people don't return to sport after ACL surgery is a fear of injuring their knee again. ***A successful outcome from rehab without surgery will mean that your knee feels great and you regain full movement and function **** it is not settling for a second-rate option. Unfortunately, some people still have knee instability (knee collapsing or giving way under them) after trialling rehab alone. For these people, there is a risk of damage to other parts of the knee. In this case, surgery is recommended to prevent further knee damage. We have grown up with the notion that ACL recons are the gold standard for getting back to sport and our previous activities. But ... there are always risks associated with any surgery, so if we can avoid unnecessary surgery and still get a good outcome – Is this not the best option? You can always get surgery if you feel your knee is not strong enough… at any time – It is not an emergency. The University of Melbourne has developed this great decision tool to help you get a non- biased opinion and the evidence surrounding the decision to get surgery or to trial rehab. https://www.aclinjurytreatment.com/treatment-options If you have any questions/ comments about your options drop it in the comments or send me a message. *this advice is general and not specific to your injury. For more information or an appointment, including telehealth, contact the practice > [email protected] #TablelandsPhysio #Lithgow #Alliedhealth #ACLrupture #ACLrehab
1 Comment
Unravelling the Mystery: How Your Neck Might Be Causing Your Headaches
Have you ever considered that the nagging headache you can't seem to shake might be caused by something other than … red wine… chocolate… hormones? The culprit could be your cervical spine- aka your neck!!. Most days I am told by someone that they have been having ongoing headaches and migraines. Many have had multiple scans and taking a lot of medication. Often this has been ongoing for years! True migraines are really debilitating. But is it always just a chemical imbalance in your brain setting off the pain? Most headaches sit somewhere on the continuum between a cervicogenic (neck) headache and a migraine. Having the option to reduce the pain by treating your neck can be game changing for people’s lives. Understanding the Cervical Spine-Headache Connection 1. The Role of Muscles and Joints: The neck is a complex network of muscles and joints. Poor posture, prolonged screen time, or even stress can lead to muscle tightness and joint irritation in the neck. This tension can result in pain that radiates upwards into your head, manifesting as a headache. 2. Nerve Pathways: The top of the cervical spine is a nerve centre, where many nerve pathways converge. If any of these nerves are irritated, they can send pain signals to your head. 3. Referred Pain: Sometimes, pain is felt in a location different from its actual source,known as referred pain. A classic example is a cervicogenic headache, where the source of the headache is in the neck, but the pain is felt in the head. What Does This Mean for You? Understanding this connection is vital, especially if you're someone who frequently experiences headaches. It opens up new options for relief and treatment. A thorough assessment and treatment by a physio to help determine the cause, changes in posture and neck exercises could make a significant difference. Taking Action If you're suffering from persistent headaches, consider it might be coming from your neck. Treatment directed at your neck might hold the key to alleviating your pain and it will be a simple way to help diagnose if your pain is a cervicogenic headache (caused by the neck). A balanced approach involving hands on treatment, exercises and professional advice can offer much-needed relief. Remember, your headache may be caused by your neck! To organise a time to assess your ongoing headaches book online or call the practice 0263523131. As we come out the other side of winter sports and dive into summer sports, now might be the time to upskill on some injury prevention programs. At Tablelands Physio, we're excited to spotlight game-changing injury prevention programs that are revolutionising athlete injury prevention and performance at all levels.
🔥 Spotlight: The Programs Pioneering Change 🔥
🧠 Mental Fortitude: The Unsung Hero The symbiotic relationship between mental and physical well-being cannot be stressed enough. A reduction in injuries not only ensures physical health but also paves the way for heightened mental resilience. As we always say, a sound mind in a sound body is the best defense against injuries. 💡 Quick Safety Tips:
As we wrap up this edition, remember, prevention is better than cure. Playing sport does not have to result in injuries. If you're interested and want to delve deeper into these prevention programs, our team at Tablelands Physio is here to assist. Stay sporty, stay safe, and see you in the next edition! Warm Regards, The Tablelands Physio Team
Are you gearing up for knee surgery? The thought of surgery can be intimidating, but remember - preparation is key. An integral part of this preparation is assembling a dedicated team of professionals, including a physiotherapist and exercise physiologist. These experts can significantly enhance your surgical outcome and streamline your post-surgery rehabilitation. So why choose Tablelands Physio? Here are THREE compelling reasons that illustrate how we can ensure a smoother recovery journey for you: 1. Personalized Prehab and Rehab Program: Every patient is unique, and so should be their recovery plan. Our experienced physiotherapists design a rehabilitation program that's tailored to your specific needs. Our focus? Strengthening the muscles stabilizing your knee and lower leg, enhancing joint range, reducing swelling, and boosting overall fitness pre-surgery. 2. Effective Pain Management Techniques: Pain management is critical both before and after surgery. Our team will equip you with various pain control strategies, including manual therapy, therapeutic exercises, and other modalities. Our goal is to empower you, helping you manage your pain and symptoms effectively. 3. In-depth Education and Continued Support: Knowledge is indeed power. We believe in empowering our patients with a comprehensive understanding of their condition and the recovery process. Our team is always here to address your concerns, answer questions, and guide you through any challenges that might arise during rehabilitation. Remember, being informed and supported translates to better surgical outcomes. Don’t face your knee surgery journey alone. The team at Tablelands Sports & Spinal Physiotherapy is dedicated to guiding you along your recovery path. Our commitment to personalized pre and post-surgery plans, innovative pain management strategies, swift rehabilitation, and thorough education makes us a trusted choice for many. Reach out to us today, and let's work together towards restoring your mobility and reclaiming your active lifestyle. Stay strong and healthy!! Every day we encounter numerous cases of knee injuries - from sports mishaps to everyday wear and tear. If you've recently experienced a knee injury, we want to assure you that you're not alone and the team at Tablelands Physio are here to help!
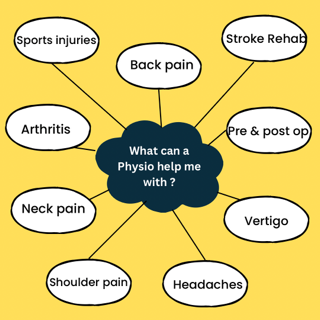
The first line of action for any knee injury is to seek a professional assessment from a physiotherapist. They will evaluate your condition and, if needed, may recommend further diagnostic procedures. A common question that arises is, "Do I need surgery?" If we think a surgical review is beneficial, we'll initiate a detailed discussion with you and your doctor. It's important to remember that not every knee injury needs surgery. Many that we have traditionally thought need surgery, such as an ACL rupture or a meniscal tear, may not require surgery. In fact, a comprehensive prehabilitation program can often help you avoid the operating room! However, if surgery is the best course, remember that knee surgery usually isn't an emergency, so you have plenty of time to explore your options and make an informed decision. Here are some proven strategies to assist your recovery: 1. Tailored Rehab Program: Let's work together to develop a program that targets strengthening your knee muscles, enhancing mobility, and decreasing swelling. A balanced approach to exercise is key - too much too soon can increase pain, while too little might hamper your recovery. 2. Nutrition: It's time to embrace a healthy diet! Foods rich in proteins, vitamins, and minerals accelerate tissue healing. Incorporate Omega-3 fatty acids to help reduce inflammation and make sure to hydrate often. Let's sideline alcohol for a while, as it can slow down your healing progress. 3. Sleep: Adequate sleep not only feels great but also significantly aids recovery. Quality sleep enhances muscle recovery, helps manage pain, and controls inflammation. So make sure you're getting those restful 7-9 hours every night. Remember, our bodies are incredible healers. With the right rehab program, nourishing diet, and ample sleep, you'll be giving your knee - and your overall health - the best chance at a speedy recovery. Let's get back to doing what we love, together! Stay strong and healthy! Physiotherapists diagnose and manage a broad range of conditions with the bones, muscles, cardiovascular system, nerves and other parts and systems of the body. They can help people to manage chronic diseases, give lifestyle advice, prescribe exercises and prescribe aids to help people manage better.
Physiotherapy also use physical techniques to improve movement, reduce pain and stiffness, speed up the healing process and increase quality of life. We have listed just a few of the areas that physiotherapists can treat. If you are interested in finding out if we can help you, get in contact with us!
Incorporating regular strength training into your exercise program has a multitude of benefits including:
Ideally, strength exercises should be completed at least twice per week, consisting of different exercises targeting all the major muscle groups. Aim to complete 2-4 sets of 8-15 repetitions for most exercises. You should have a couple of repetitions in reserve at the end of each set, if you are struggling to reach the number of reps you aimed for you need to make the exercise easier, and if you could easily do 5 or more reps than you did, it is time to make the exercise harder to ensure you continue to challenge the muscles and make progress. If you don't have weights at home you can use anything from around the house; A backpack/shopping bag filled with items, big bottles of water or even just a brick. ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au
Do you have exercise and activity related goals you need help achieving? We have a highly qualified team of Exercise Physiologists and Physiotherapists who are experienced working with NDIS clients to help them achieve their goals.
This may be to increase strength, to get out and do the shopping, be able to walk up and down the stairs or even just gaining confidence to get out and about. We work with so many different people and individualise their programs to their goals in a fun and creative way. Pictured in the video is little superstar, Noah, who was referred to us to help regain his strength, coordination and confidence. He has been working hard alongside Physiotherapist, Mali to achieve these goals. Please don’t hesitate to get in contact if you have any questions. ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au Sometimes we worry about what’s wrong with our bodies, we feel a sharp pain, a tweak, or an ache in our back (or neck), then we panic, stop moving, and start googling. This can be unhelpful and it’s so hard to know what the right thing to do is… Do you need to go to Hospital, the Doctor, the Physio, Chiro, the massage guy, a specialist? Often, you’ve just over stretched or put yourself in a position that your body wasn’t happy to be in. These are the things I hear every day. “It’s out “ “It’s tight “ “It’s stiff” “I’m weak” “It’s damaged” The Dr said “It’s bone on bone” “Irreversible damage” “Old age” “Riddled with arthritis” We need to have something to blame for the pain. Combined with the stress and implications….. “I can’t sleep” “I can’t play sport “ “I can’t work” “I can’t travel” “I can’t play with my kids” “I’ll have pain for the rest of my life” These thoughts and stresses all contribute to your amount of pain and how long it will last for. Chances are it isn’t as bad as you thought initially. Unless you’ve done something crazy like fallen from a tree, crashed your car, been squashed in a footy scrum and even then, most people are fine (this obviously depends on how high up the tree you were). If we are talking backs, there are a few things that might help you to know:
So, what to do?
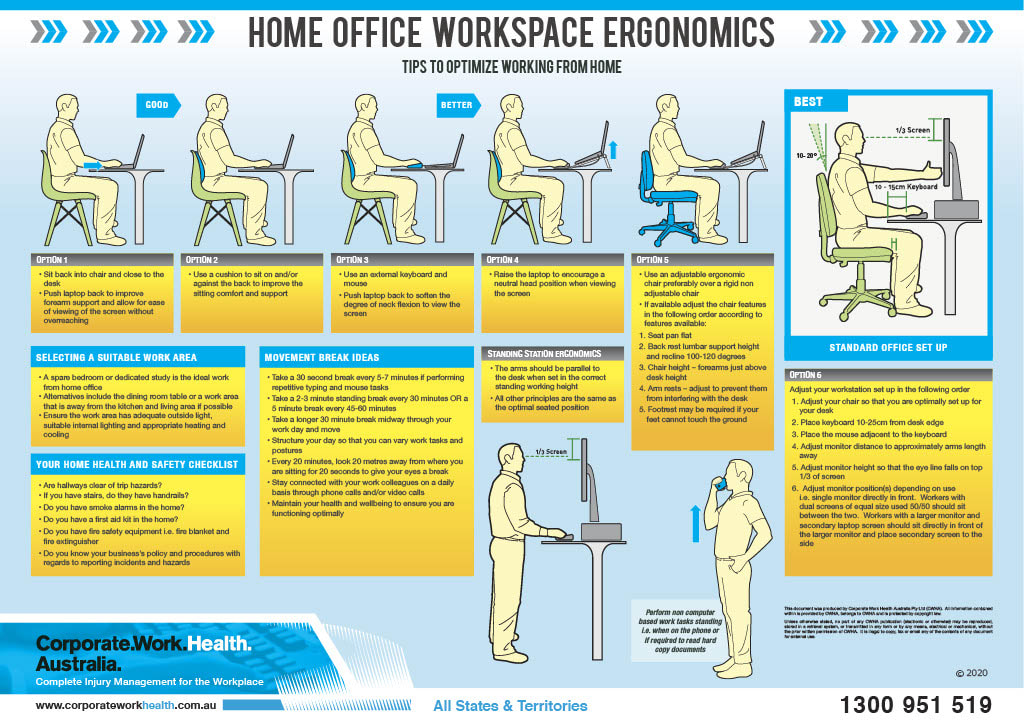
Sal’s 10 step plan: 1. Relative rest, (not bed rest) is best for a couple days, hot water bottles are lovely, regular anti-inflams/Panadol (if you can take these) - keep changing positions, try and keep any pain in your leg at a minimum, some gentle walking if you can, is also good idea. 2.You are generally better to lie down for a short rest than hang out on the lounge or recliner. Positions that lessen the leg pain are better. 3. Gently try and get moving. Back movements are good and won’t cause any damage. Lie on your tummy if you can and come up onto your elbows. Using a heat pack can help make this easier. Just lie there for 10 mins if you’re feeling ok. Up and down a few times over the time. Or try lying on your back and rolling your knees side to side. 4. Any position/stretch that lessons the leg pain or gets better after you do a few, then they are the ones to start with – little and often rather than a stack, then nothing. You can’t hurt yourself doing these. All the gentle movement is fabulous and helps to move any inflammation and swelling away. 5. Know that it will get better. 6. Pain is an interpretation of signals sent to our brains - messages are sent from the back to the brain. People in pain have their brain “lit up” on scanning. The inputs from the back is just one of these lights. There is a whole back pain network in your brain. Other things that contribute to “lighting up your brain” include other stresses, anxiety, depression and frustration. Things that improve or reduce this brain sensitivity are things that make you happy, calm, and less stressed. Change any of these more negative emotions to a positive one and aches and pains can reduce. Control what you can and let the rest go. 7. All pains and injuries involve the immune system. Pain can cause your immune system to become a bit out of balance. Anything that is good for the immune system will help your body cope with the pain. Immune healthy behaviors include working out ways to cope, graduated exercise, anti-inflammatory foods, laughter, sleep well, any interaction with nature, less alcohol (a glass of wine is ok, just not a bottle) and avoid drugs with opioids in them (these can make you more sensitive over time). 8. Challenge your perception about how bad it was initially 9. Seek the knowledge and treatment that will provide you with a well-rounded program including ways to reduce your pain, exercises, self-management strategies and advice to get you back doing the things you love, as soon as possible. The correct team of health professionals around you and supporting you is invaluable. (They will also help you with the correct plan of attack if things are not going to plan) . 10. Did I mention … Keep Moving? If this helps you or raises more questions, we are always here to answer questions and help you decide the correct treatment pathway. Look after yourself. Sally APA Musculoskeletal Physiotherapist Director, Tablelands Sports & Spinal Physiotherapy ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au *** Please note this is generalised advice for people with back pain, not specific to your case. Please contact your local physio or healthcare professional if you are concerned about any of your symptoms or if they are increasing. The quicker you get on top of this the better. *** In Australia at any one time, 25% of the population report low back pain and 20% report neck pain. A large proportion of people are working in front of a computer– even those “active” tradies. Combine this with many more working from home, it’s no wonder that we are treating a large proportion of people with headaches and back and neck pain – often associated with increased sitting. Our bodies are not designed to sit and be static for long periods, but many peoples work demands (and Netflix addiction) means we are sitting more. This is a list of things you can do to help you cope with too much sitting. Remember the main thing is our bodies like movement, regardless of how good our desk set-up is.
Some Extra Tips: a) Eyes - Look 20 metres away for 20 seconds every 20 minutes (20,20,20 rule). b) MOVE – get up and move every hour for 5-10 minutes and have a minimum 30minute break at lunch time c) Try to go for a 30 minute walk every work day - your body and brain will love you for it. Sally APA Musculoskeletal Physiotherapist Director, Tablelands Sports & Spinal Physiotherapy ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au If you have a loved one who lives with chronic pain, one of the most important things you can do is ensure that they feel connected. Invite them to events, and accept that when they can’t come, its not because they don’t want to. Find ways to be involved in their life without increase the demands on the body.
Be understanding that some days they may have greater capacity than others. Do not judge them by their good days, and don’t exclude them based on their bad days. Just remember, its not about trying to fix them; its about helping them to connect to the world around them, helping them to feel involved and returning to them a sense of control. As a healthcare professional, how can I help a patient who suffers from chronic pain? By building a connection with them. By developing a relationship based on trust and understanding that helps the patient to feel more in control of their pain, their body, and their future. If you are suffering from chronic pain and are feeling disconnected, visit the Chronic Pain Australia website https://chronicpainaustralia.org.au/ or look them up on social media. We would also love to see you in the clinic where we can help you to learn more about how you can regain control of your pain, so that you can return to doing the things you love, with the people you love. Amalia Rawson Physiotherapist B.Physio ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au In life we are connected to many things at different times. Our most meaningful connections come from our friends and family. Unfortunately, for those with chronic pain, these connections can feel damaged. Pain can make you feel isolated or lonely. This can be both real or perceived and only becomes more common with age, just as rates of chronic pain increase with age.
A sense of connection is vital for those suffering from chronic pain. Being in a constant, or near constant state of pain decreases opportunities for social interaction and involvement in group activities. Often this can be due to a lack of understanding from friends and family as to how pain impacts an individual’s life and function. It can be very challenging to understand how it feels to live with chronic pain if you have not experienced it. This loss of understanding leads to feelings of isolation: from the community, from friends, and even from family. People with chronic pain often feel as though they should just ‘get over it’ or ‘push through the pain’. However, this often only leads to an increase in pain and further isolation. This feeling of disconnect is also common when seeking professional help. Its not uncommon for people with chronic pain to feel ostracised or dismissed by the medical community. For effective treatment of chronic pain conditions and disorders health professionals need to understand the importance of connection in treatment. That is connection between themselves and the person in pain, as well as connection to other members of the healthcare team; always with the patient at the centre, calling the shots. Another level of connection that is important when talking about chronic pain is a person’s connection to their own body and psychological state. Its important to develop an understanding of our own pattern of pain. Knowing exactly much you can do without causing a flare up of pain is a vital part rebuilding connection with others. It can also help to provide you to build your ability to own your pain, rather than letting your pain own you. People suffering from chronic pain can feel like they have no control over their lives. Gaining a better connection and understanding of their pain can help to return a sense of control to those who may have felt that they had none. Amalia Rawson Physiotherapist B.Physio ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au We all know someone who suffers from chronic pain. 1 in 5 Australians suffer from it with that number increasing to 1 in 3 over the age of 65. Chronic pain conditions include many diagnoses; from those widely recognised with clear bio-mechanical causes such as; arthritis (osteo and rheumatoid), osteoporosis, MS, nerve damage, etc; to those we are rapidly developing our understanding of like chronic lower back pain, and polymyalgia rheumatica; and those whose causes still largely mystify the medical community: fibromyalgia, chronic fatigue syndrome, chronic regional pain syndrome.
It is generally considered chronic, or persistent pain, when it lasts for more than 3 months, or longer than the tissues would normally take to heal. Chronic pain is felt differently by every person. It can be mild or quite severe, sharp or blunt and achy. For most people with chronic pain, it is felt on most days and can very in intensity depending on how much and what type of activity the individual does on that day. As we mentioned in the previous blog, pain signals are carried by nervous system to the brain to indicate danger and/or damage. This isn’t always the case with chronic pain. During chronic pain, our body will send these pain signals even though there is no risk to tissues or long after the initial injury has healed. Sometimes these pain signals even get mixed up and start coming from a different part of the body to where the initial injury was located. With this sort of pain, it is important to have a multidisciplinary approach. This means involving more than one type of healthcare professional in a person’s care. As more than 40% of chronic pain patients admitted to hospital with chronic pain have a diagnosis involving the muscles and/or bones, physiotherapists are often a key member of the multidisciplinary healthcare team for chronic pain. Studies have also shown that a graded approach to exercise can be crucial in decreasing pain, increasing function, and improving an individual’s quality of life. Chronic pain can be like a roller coaster where an individual will feel good one day and terrible the next. This often occurs when someone feels well and tries to get as much done as they can whilst they feel well…only to over do it and be in intense pain the next day. This becomes a roller coaster of pain and dysfunction. One of the most effective treatments for this pattern of pain is graded exercises. This involves first discovering how much exercise or other work they can do without suffering from a flare-up soon after. Using this as a baseline, we can very slowly increase the amount of exercise that a person can tolerate before flare-up. This technique has proven to be very effective when accompanied by education and advice of a trained healthcare professional. Or better yet, a team of trained healthcare professionals. Amalia Rawson Physiotherapist B.Physio ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au Acute pain: Causes and treatments
Pain is a message sent via the nervous system from an injured body part to the brain. This pain signal usually signals to the brain that the body’s tissues are being damaged or are in danger of being damaged. Acute pain is caused by damage to the tissues through injury, inflammation or an active disease process. Acute pain generally passes as the affected tissues heal and rarely lasts longer than 3 months. The rate of healing, and therefore pain reduction, is dependent on which tissue is damaged. Causes of acute pain include things like
During a period of acute pain, it is important to be fully assessed by a professional to ascertain the cause of your pain and commence treatment as soon as appropriate for your injury. This will ensure that an acute injury does not later become chronic pain. Amalia Rawson Physiotherapist B.Physio ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au An INTRO TO PAIN
Today we kick off the beginning of National Pain Week. Over the course of the following week, we will be releasing a series of blogs centring around pain and its many causes and dimensions. This year the topic for National Pain Week is CONNECTION. Pain, and especially chronic pain, can lead to increased levels of social isolation. The aim of National Pain Week this year is to bring awareness of the impact that social isolation has on those suffering from persistent and chronic pain. We particularly want to remind family, friends and health professionals just how powerful connection can be for those suffering from chronic pain. Pain is defined as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage" by the International Association for the Study of Pain. Pain is not the simple, straight forward process that we often think it to be. It is diverse and can mean many different things to different people. We generally think of pain as our body’s way of saying ‘STOP’ or ‘DAMAGE’. This is true of acute pain, but in chronic, or persistent pain, this isn’t always true. Sometimes it is simply our body’s way of saying ‘I’m scared’ or ‘last time we did this it hurt’. In these situations, the body may benefit from gentle re-education, under the guidance of a trained professional. Follow us over the next week to learn more about the differences between acute and chronic pain, how they can be treated effectively, the importance of connection, and how you can help someone suffering from chronic pain. Amalia Rawson Physiotherapist B.Physio ☎️ 6352 3131 ✉️ [email protected] ℹ️ www.tablelandsphysio.com.au |
Copyright © 2024 All Rights Reserved - TABLELANDS SPORTS & SPINAL PHYSIOTHERAPY
177 Mort Street Lithgow NSW 2790 : Tel: 02 6352 3131 : i[email protected]
Click here to view our Privacy Statement | Click here to take our Customer Satisfaction Survey | Click here to read our Complaints Procedure | Click here to view our Terms & Conditions
177 Mort Street Lithgow NSW 2790 : Tel: 02 6352 3131 : i[email protected]
Click here to view our Privacy Statement | Click here to take our Customer Satisfaction Survey | Click here to read our Complaints Procedure | Click here to view our Terms & Conditions